Artificial intelligence (AI) has enormous potential in healthcare, but all too often, it gets misunderstood. Especially with the proliferation of AI in other industries and chatGPT.
And yet, AI offers more promise than that. With the right supporting infrastructure and context, intelligent tools stand to not only pump out data but also tangibly improve diagnostic and therapeutic decision-making at the point of care. In turn, AI can help identify more patients for biopharma companies—and faster, too.
Really. Consider, for example, early detection. Pharma-sponsored AI solutions are known to evaluate large and diverse data sets like EHR and imaging data at scale and predict in real-time when something’s wrong such as a stroke, heart attack or rare event that doctors otherwise wouldn’t look for.
But the clinicians still must act, which can sometimes be the hardest part. In turn, the best AI tools are those that combine the algorithm with care activation, which alerts clinicians and then integrates care recommendations into clinical workflows. Done right, this potent combination can transform AI into something much more powerful than analytics and algorithms alone.
Why care activation matters
Generally, the more nuanced the disease, the more complicated the patient journey. Up to 10% of patients with rare diseases don’t have a diagnosis at all, for example. If they ever get one, it may take up to 4 to 5 years, on average.
The physicians doing the diagnosing are passionate and skilled but also frequently overworked and overburdened. That’s why they’ve increasingly welcomed AI decision support, such as medical documentation or other automations that make their jobs easier. Algorithms that alert clinicians to possible new diagnoses are another breed of tools that could help narrow care gaps—if those tools get built with integration in mind.
“What really drives doctors’ adoption of technologies, AI included, is the ability of that technology to be integrated into their workflows,” said Bernice Ma, Principal at Evolution Road, a commercial impact strategic consultancy “New technology shouldn’t require significant incremental effort to use or learn.”
Despite the crowded market of AI-supported clinical tools, though, the care activation piece often gets overlooked. Vendors can get preoccupied with their own tech’s capabilities, Ma said, without paying enough attention to how the tool fits into daily practice.
“But that’s the most important part,” she said. “The algorithm is not enough to drive adoption. Care activation requires that doctors are alerted to what’s wrong, and then have a system in place to coordinate care from there. Taking action must be easy and seamless.”
AI and early detection in practice
The more providers see what AI algorithms plus activation can achieve in the clinic, the more they’re relying on that combination as a detection aid. Viz.ai, for example, already has algorithms running 24/7, coupled with purpose-built care activation in more than 1,400 hospitals with 35,000 HCP users, who quickly take action (1 patent every 13 seconds) on the AI recommendations, directly from their workflow. That footprint is leveraged by manufacturers, who sponsor the development of new algorithms—often as part of their commercial marketing and medical strategies.
Thanks to that partnership from pharma companies, physicians across therapeutic areas now have decision support they didn’t before. Complex specialties such as cardiology and neurology are currently seeing the most traction, but Ma expects other fields to embrace AI too.
“The technology is possibly seen as the most valuable in disease areas where finding the patient in a timely manner becomes really important to outcomes,” she said. “So naturally, you’re seeing a lot of interest in cardiology, neurology and even rare diseases and oncology, which all involve a lot of labs, data and coordination before you can appropriately diagnose patients.”
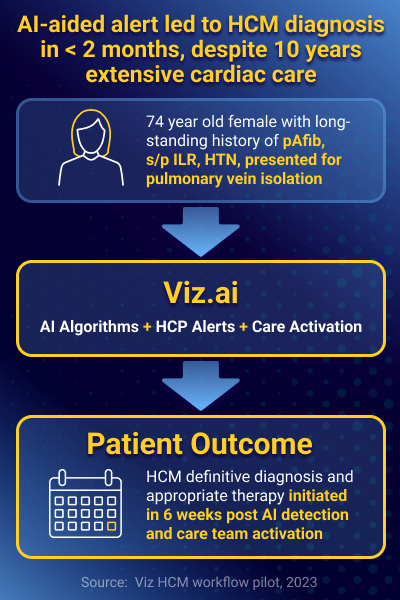
Viz.ai has an established algorithm and activation program for stroke, which has led to lower rates for length-of-stay and disability. More recently, the company received de novo approval for hypertrophic cardiomyopathy (HCM), a rare and usually hereditary condition that affects 1 in 500 people. With that program, a 74-year-old patient finally got the right HCM diagnosis within just three months, after having her condition go undiagnosed for 10 years despite extensive cardiac care.
These use cases are just the start, Viz.ai says. Potential future applications include transthyretin amyloidosis and pulmonary hypertension, as well as other areas that have a similar need for early detection and improved care pathways.
Giving AI what it needs to transform
With a world of promise at the point of care, algorithms are certainly beneficial in the clinic. But they’re also relatively useless without a way to activate HCPs. By incorporating a mechanism for care activation into the platform, it can take the tool to the next level.
Because indeed, algorithms plus activation are a potent combination that can accelerate diagnostics and treatments, optimize clinical efficiencies and improve patient outcomes—plus, of course, find new markets for manufacturers to explore.