 |
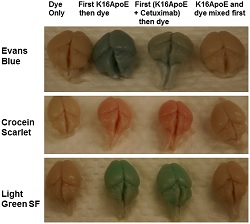
| Three different dyes as used alone, with K16ApoE and with K16ApoE and the cancer drug cetuximab--Courtesy of Mayo Clinic |
The blood-brain barrier is the body's method of keeping harmful substances away from the brain, but it's also a daunting obstacle for drug delivery experts looking to shuttle treatments there. Now, researchers at the Mayo Clinic have developed a synthetic peptide carrier to shuttle small molecules past the barrier and into the brain.
As published in the journal PLOS ONE, the scientists injected the synthetic peptide K16ApoE intravenously into mice. The peptide binds to proteins in the blood, the combination of which is recognized by receptors on the blood-brain barrier and allows for its natural, passive transport into the brain.
In the study, the team successfully delivered 7 different small molecules to the brain, including cancer drugs cisplatin and methotrexate. They also experimented with an eighth molecule: insulin, which suggested that the method of ligand-receptor signaling is "a natural means for passive transport of some molecules across the BBB," according to the abstract. And for the sake of illustrating brain uptake, they used a series of colored dyes to show to what degree the molecules had bypassed the blood-brain barrier.
"Not only have we shown that we can transport 8 different molecules, we think this method will be less disruptive or invasive because it mimics a normal physiological process," study author Gobinda Sarkar said in a statement in an announcement from the Mayo Clinic.
Crossing the blood-brain barrier is one of those notorious holy grails in drug delivery, and there's a wide-open market for a platform that could help deliver drugs for brain cancers or Alzheimer's disease, for example. Among those working on a "piggy-backing" model similar to the Mayo Clinic's are MedImmune, which in March partnered with Canada's Bioasis for their p97 protein shuttle; and Roche ($RHHBY), which dropped its BACE inhibitor program for Alzheimer's but touted a study earlier this year demonstrating a delivery method using the transferrin receptor pathway to ferry antibodies into the brain for the same disease.
"We know that some chemotherapeutic agents can kill brain tumor cells when they are outside the brain (as in a laboratory test)," lead author Robert Jenkins said in a statement. "But because agents cannot cross the blood-brain barrier, they are not able to kill brain tumor cells inside the brain. With the peptide carrier, these agents can now get into the brain and potentially kill the tumor cells."
- here's the Mayo Clinic report
- and here's the PLOS ONE abstract